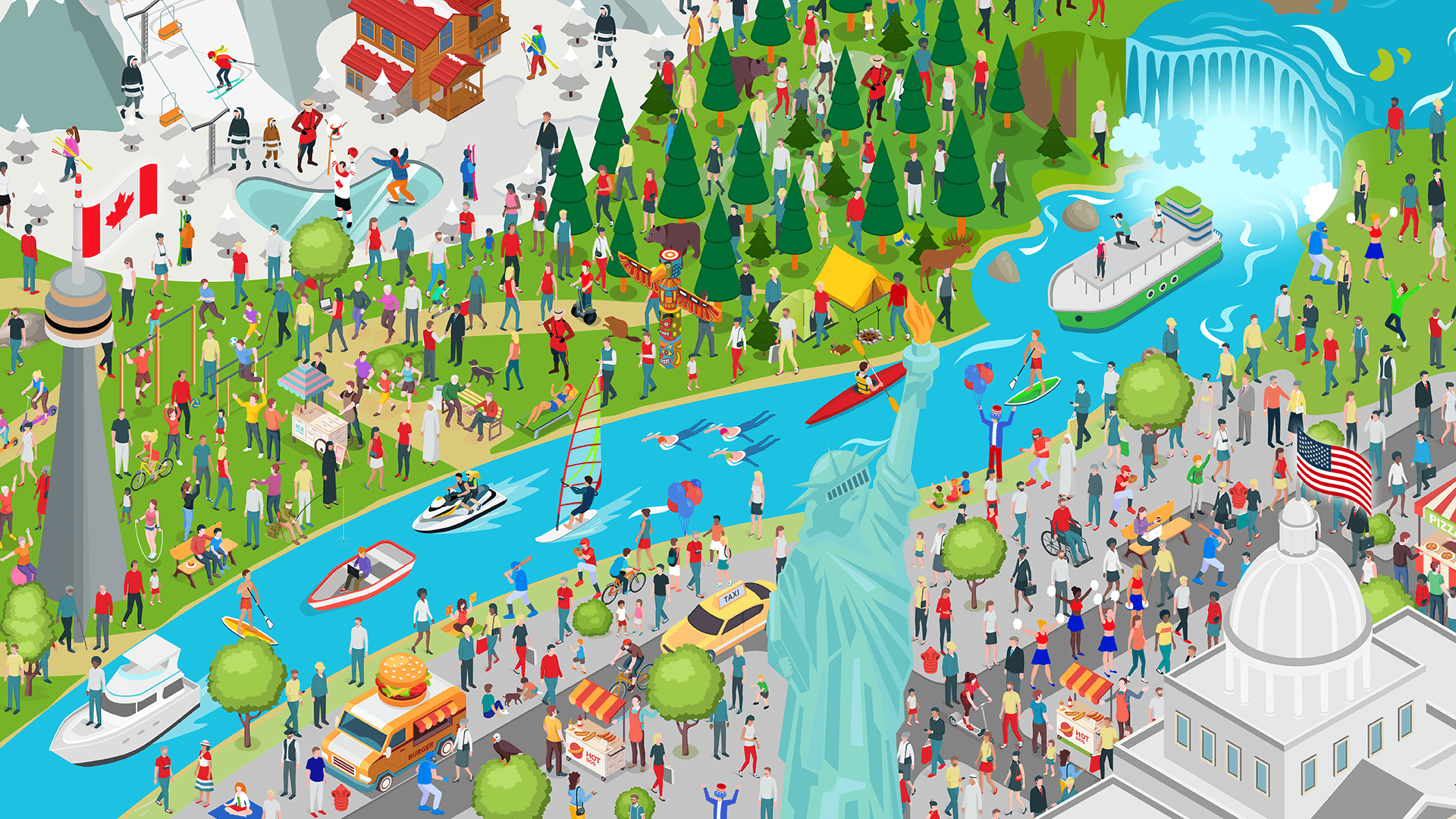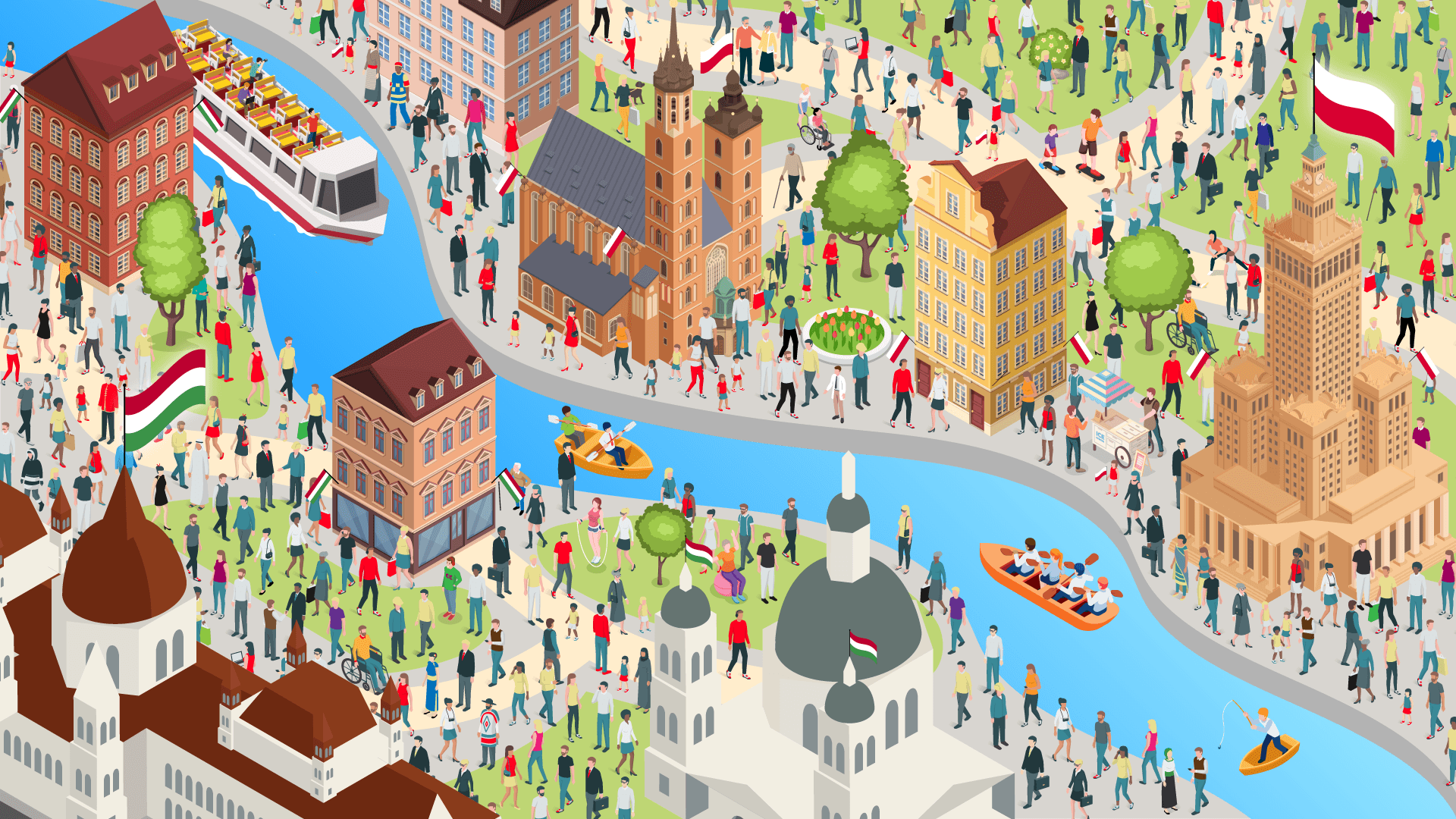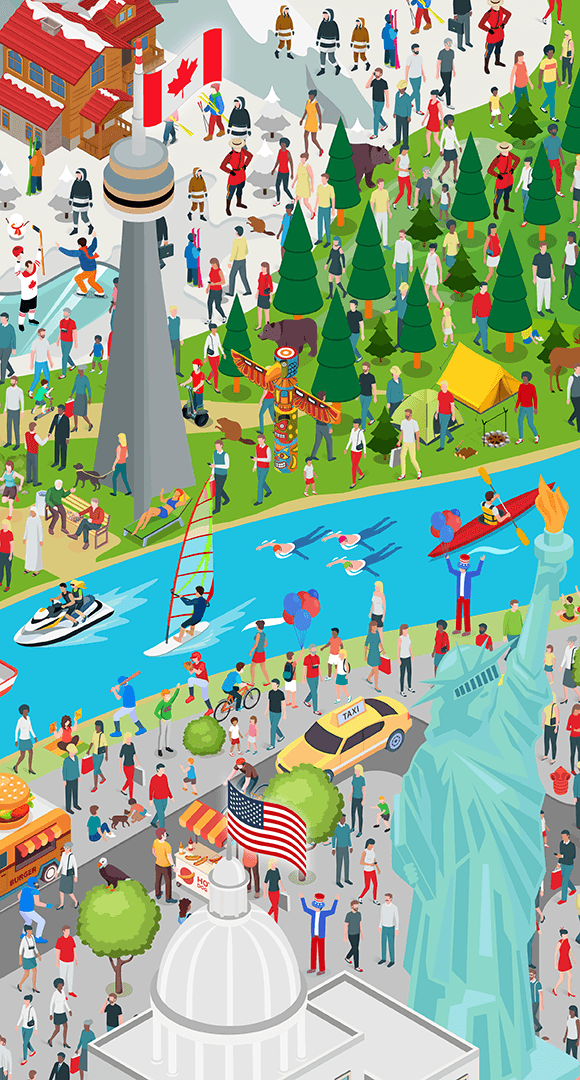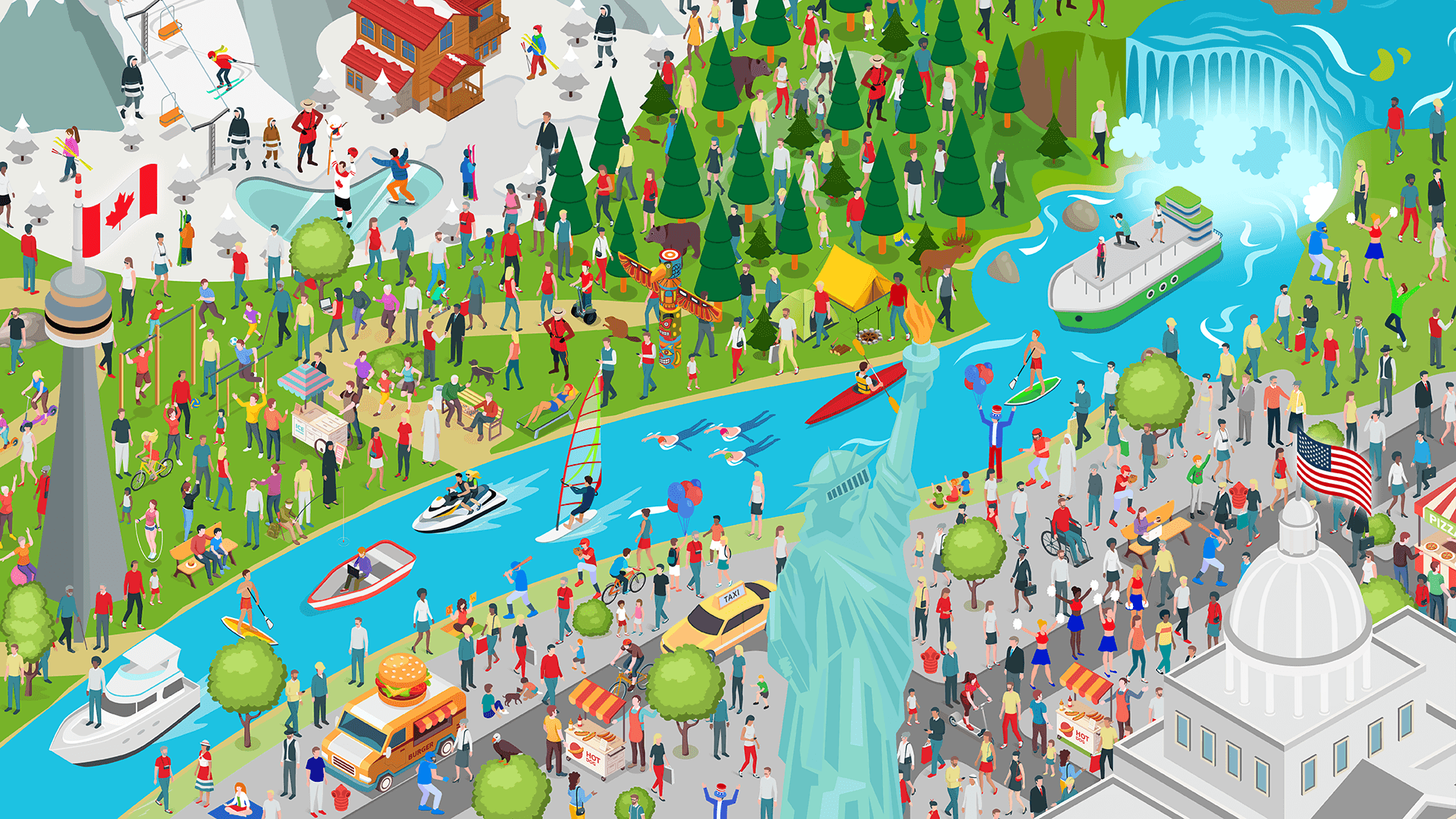
Where’s Crohn’s & Colitis (CC)?
Inflammatory bowel disease (IBD) is a global health challenge1 that has no borders. Join us on an adventure across borders as we work towards a sustainable future with equitable IBD care.
It’s simple – you just need to ask Where’s Crohn’s & Colitis (CC)?
Find the CC characters wearing green t-shirts in the different locations on our map to discover how access to care and treatment can vary for people living with IBD, the impact this has and what solutions there are from a global perspective.
Large parts of the US and Canada are rural and sparsely populated, so hospitals with specialist clinicians are often long distances apart.2 This means some people with IBD, depending on where they live, have to travel many hours and even stay overnight to receive hospital treatment.














About the Where’s CC? campaign
Celltrion is committed to shining a light on unseen inflammatory bowel disease (IBD) patients to overcome inequalities in access to treatments and quality care across the world.
IBD is often considered an invisible illness12. We are on a mission to make people look beyond what they would usually see, to make all people living with IBD seen.
The Where’s Crohn’s & Colitis (CC)? campaign aims to spark conversations about inequalities to drive change in clinical practice and empower all people living with IBD to advocate for themselves.
For World IBD Day 2024, Celltrion launches the second installation of the Where’s CC? campaign, focusing on inequalities in access to treatments and care at a global scale.
In 2023, Celltrion partnered with the European Federation of Crohn’s & Ulcerative Colitis Associations (EFCCA) for World IBD Day to spotlight age-based inequalities in IBD in the first installation of the Where’s CC? campaign.
As inequalities grow at a global scale, urgent action is required to ensure sustainable and equitable IBD care for all.






About IBD
IBD is an umbrella term used to describe conditions including Crohn’s disease and ulcerative colitis. Collectively, IBD impacts over 10 million people worldwide with incidence rates rapidly increasing across the world13.
IBD is a long-term condition and there may be times when the symptoms are severe, known as a flare-up, and times when there are no or few symptoms, known as remission. Common symptoms of IBD include pain, cramping or swelling in the stomach, episodes of diarrhoea, weight loss and extreme tiredness14.
IBD can appear for the first time at any age, however, diagnosis most commonly takes place between the ages of 10 and 4013.
Treatment for IBD can be transformative for patients’ lives, reducing the impact of the condition on their lives by minimising flare-ups and maintaining remission.
In recent years, the increasing availability of new treatments has transformed IBD patient care. Innovations in treatments, including advances in treatment administration that enable people to access at-home injectable treatment (versus hospital-based treatment), allows people to have an improved quality of life whilst managing their condition15.
People with IBD often have to commit to a treatment for years, so it’s important for healthcare professionals and patients to work together to find the best treatment for them. Increasing our clinical understanding of IBD will support this and ensure that every person with IBD is empowered to overcome the condition and its symptoms.



Inequalities in IBD
There is growing evidence that people living with IBD are experiencing inequalities in access to care and variations in their experiences and outcomes.
Inequalities are complex and several factors may influence whether somebody is subject to inequitable care, including16:
-
Socioeconomic status
-
Ethnicity
-
Gender
-
Age
-
Geographic location
-
Awareness and education
-
Comorbidities
-
Clinical research
-
Health system limitations
-
Language and cultural barriers
Inequality affects outcomes, access and experience in IBD care. This is due to groups of people being unable to access innovative treatment options, experiencing a disproportionate impact of the disease on their day-to-day lives, having a long wait to receive a diagnosis and not being involved in decisions about their care16.
The rising burden of IBD globally is anticipated to worsen inequality in access to high-quality IBD care and the affordability of IBD care for health systems1.



IBD has no borders
IBD is now defined as a global health problem, as an issue that transcends national boundaries that needs to be addressed through collaboration1.
Access to care and treatment is variable across the globe and even within countries, impacting people’s experience of care and ultimately their outcomes16.
We urgently need to raise awareness of the inequalities that exist in IBD to drive collective action to tackle the root cause and empower people living with IBD to advocate for the best possible care, no matter where they are in the world.
By increasing access to a timely diagnosis, high quality care and innovative treatments, we can ensure sustainable and equitable IBD care globally.






IBD has no age
IBD has no age – but the clinical research and general awareness of the condition do not reflect this17.
From teenagers to elderly people, a lack of understanding and research in specific groups of people are leaving them unable to benefit from innovative treatment options, and therefore feeling isolated18.
By addressing these challenges, we can ensure ALL patients, no matter their age, have the opportunity to benefit from potentially life-changing treatments that work for their condition, but also their lifestyle.


Real life stories
Hear from leading IBD clinicians on the challenges in access to IBD care, and how improved treatment options and awareness can support in improving people’s quality of life.
Diagnostic Delays
Delayed and inaccurate diagnoses preventing early and effective disease management 19.
Healthcare Infrastructure
Health systems with insufficient resources and tools resulting in poor IBD treatment outcomes 19.
Geographical Disparities
Limited access to specialised IBD care and professionals in remote or underserved areas resulting in treatment delays or insufficiency 19.
Financial Barriers
High healthcare costs, inadequate insurance and costs associated with seeking care leading to people avoiding or discontinuing IBD treatment 19.
Patient support
If you think that you or your loved one could have IBD, or you have a diagnosis and are concerned you are not accessing the best possible care or treatment for your IBD, speak to your local doctor.
No matter your circumstance, it’s important to work closely with your doctor to get an appropriate diagnosis and find a treatment that is clinically effective whilst being suitable for your lifestyle and personal priorities.
To help you get the best support, try these simple approaches:
1
Be open and honest with your doctor about your symptoms and how these are impacting your day-to-day life.
It may seem small to you, but it could be the key to unlocking a diagnosis. Before your appointment, keep track of your symptoms and how these change over time. Think about what you want to get out of a treatment.
2
Once you have a diagnosis, discuss the range of treatment options available to you and their pros and cons with your doctor.
Helpful prompts for your appointment include; What are my options? Are there any other options that you haven’t mentioned? What are the risks and benefits of that option? Which treatment would you recommend based on my lifestyle? Which treatment is most effective for people like me?
3
Reach a decision together with your doctor.
Make sure to share your priority outcomes for a treatment, for example avoiding frequent hospital visits or addressing a particular symptom. Don’t be afraid to ask for clarification if you don’t understand any of the options.
4
If you do not feel seen and understood by your doctor, you can always ask for a second opinion.
You can ask your doctor directly to see a specialist or another doctor. If you don’t feel you can do this, look for a local patient support group – or reach out to patient advocacy groups such as EFCCA at www.efcca.org.
WANT TO PLAY WHERE’S CC 2023?
CLICK HERE TO PLAY LAST YEAR’S GAME
This website uses cookies to ensure you get the best experience on our website. By using our website, you agree to our legal policies. Privacy and legal notice.
ContinueLegal Notice
Celltrion, Inc., ("Celltrion") maintains this website.
By using this website, you accept the information, products, and services provided herein "as is" and you acknowledge that neither Celltrion, nor their agents, affiliates, partners, or licensors are providing the information, products, and services for the purposes of supplying you with medical advice because the material on this site is intended only as informational or as an educational aid and it is not intended to be taken as medical advice.
This website is for general informational and educational purposes, and it is not country specific.
Celltrion makes no express or implied warranty regarding the accuracy, content, completeness, reliability, operability, or legality of information contained within this website, including, without limitation, the warranties of merchantability, fitness for a particular purpose, and non-infringement of proprietary rights.
You should not rely on the materials in deciding on a treatment plan, drug usage, or any other medical advice regarding the materials, and Celltrion firmly urge that you consult with a licensed physician in connection with any and all treatment options that may be available to you.
By your access and use, you accept, without limitation, the terms of our Legal Notice and Privacy Policy. You are solely responsible to comply those terms and regulation in your country. Celltrion is not responsible for access to any such information which does not comply with applicable legal process, regulation or usage in your country of origin.
In no event shall Celltrion, or its agents, affiliates, partners, or licensors be liable for any direct, special, indirect, incidental or consequential damages or any damages whatsoever resulting from loss related to the use of our websites, whether in an action of contract, breach of warranty, negligence, or other tortious action arising out of or in connection with the use of the materials contained on this website.
Unless otherwise indicated, all details, documents and presentations published on our website are under the sole ownership of Celltrion. We grant you a non-exclusive license to use this website solely for your personal, non-commercial use only unless you have written consent from Celltrion for commercial use. You are solely responsible for the use of our website or contents.
Privacy Policy
Introduction
This Privacy Policy is provided by Celltrion, Inc., (hereinafter "Celltrion" or "we") and its subsidiaries/branches to explain who we are, how we collect, share, and use personal data about visitors of our website (hereinafter "you" or "user"), as well as how visitors can exercise their privacy rights. If you have any questions or concerns about our use of your personal data, or would like to exercise any of your rights — including, but not limited to, objecting to the processing of your personal data in the ways that we describe here — then please contact us using the details provided at the end of this Privacy Policy.
Celltrion does its best to protect your privacy rights.
Who We Are
Celltrion is a global pharmaceutical company headquartered in Incheon, Republic of Korea. For more information about us, please visit our website at https://www.celltrion.com/en-us
Personal Data
We do not require registration to visit our websites. However, some services may require visitors to provide us with Personal Data, such as contact details and interests.
"Personal Data" may refer to any data that identifies one as an individual or relates to an identifiable individual, such as:
• Contact details (name, telephone numbers and email addresses);
• Interests (health conditions, specific requests made through the website).
More information on personal data we collect can be found below in specific sections of Cookies Policy.
How we use personal data
We use Personal Data in order to maintain functionalities on our websites such as:
• Providing customer service to users;
• Responding to user inquiries and fulfilling any user requests;
• Sending administrative information to users, such as changes to our terms, conditions, and policies, as well as market information that we believe may be of interest to you.
We also use Personal Data to ensure that our business operations comply with any relevant legal obligations and match our legitimate interests.
Our business activities may include:
• Data analysis;
• Internal data audits;
• Identifying usage trends for our websites;
• Detecting, preventing, and investigating fraud in the use of our websites;
• Cyber security monitoring;
• Developing, enhancing, or modifying our products and services;
• Validating users' ability to access or utilize our products and services;
• Understanding how our products and services impact you and those in your care;
• Expanding our business network and scale of operations.
The Personal Data that you and other website users provide may be aggregated. We may use and disclose such aggregated data for any purpose. Aggregated data does not personally identify you or any other individual.
How we disclose personal data
We disclose Personal Data to third parties as follows:
• Our subsidiaries and affiliates worldwide for the purposes described in this Privacy Policy.
• Service providers in order to provide services including, but not limited to: website hosting, data analysis, information technology, infrastructural provision, customer service, email delivery, and auditing.
• Other companies with whom we collaborate regarding particular products or services, including our co-promoting partners for products that we develop and market jointly.
We also disclose your Personal Data as we believe to be necessary or appropriate:
• (i) To comply with applicable law, as well as our regulatory monitoring and reporting obligations (including laws outside your country of residence), (ii) to respond to requests from both public and government authorities (including authorities outside your country of residence), (iii) to cooperate with law enforcement, or (iv) for other legal purposes.
Legal basis for processing personal information (eea visitors only)
If you are a visitor from the European Economic Area, our legal basis for collecting and using the personal information as described above will depend on the personal information concerned and the specific context in which we collect it.
However, we will generally collect personal information from you only where we have your consent to do so, or where the processing is in our legitimate interests and not overridden by your data protection interests or fundamental rights and freedoms.
If we ask you to provide personal information to comply with a legal requirement or for contacting purposes, we will make this clear at the relevant time and advise you whether or not the provision of your personal information is mandatory (as well as of the possible consequences of not providing your personal information).
Similarly, if we collect and use your personal information in reliance on our legitimate interests (or those of any third party), we will alert you and clarify what those legitimate interests are at the relevant time.
Individual rights
On some of our websites, you have the option to update your profile online.
If you would like to request to review, correct, update, suppress, restrict, or delete Personal Data that you have provided us through these websites, or if you would like to request to receive an electronic copy of your Personal Data for the purpose of transmitting it to another company, you may contact us as indicated in the “CONTACT US” section. We will respond to your request promptly, in compliance with applicable laws.
In your request, please let us know what Personal Data you would like to have changed, whether you would like to have it suppressed from our database, or set certain limitations on our use of your data. We may need to verify your identity before implementing your request. We will try our best to respond to your request as soon as reasonably practicable.
When asked to provide Personal Data, you may decline. However, choosing not to provide necessary information may limit our ability to supply you with requested services.
Please note that we may need to retain certain types of Personal Data for record keeping purposes.
Data security
We seek to use reasonable organizational, technical, and administrative measures in order to protect your Personal Data. This includes encrypting your personal information in transit and at rest.
Data retention period
We will retain your Personal Data for as long as needed or permitted in light of the purpose(s) for which it was obtained and as outlined in this Privacy Policy.
When we have no ongoing legitimate business need to process your personal information, we will either delete or anonymize it or, if this is not possible (for example, if your personal information has been stored in backup archives), then we will securely store your personal information and isolate it from any further processing until it can be safely deleted.
International data transfers
Your personal information may be transferred to, and processed in countries other than the one in which you are resident. These countries may have data protection laws that are different from the laws in your country.
The servers of this website are located in the Republic of Korea (South). We may transfer your personal information with legitimate purpose to our subsidiaries/affiliates, third party service providers, and business partners located around the world.
However, we have taken appropriate safeguards to ensure that your personal information will remain protected in accordance with this Privacy Policy. This includes implementing the European Commission's Standard Contractual Clauses for transfers of personal information between our group companies, which requires all group companies to protect personal information they process from the EEA in accordance with the European Union data protection laws.
The Commission’s adequacy decision recognizes that Republic of Korea has essentially equivalent levels of protection for personal data, and transfers to Republic of Korea can be made as if they were transfers to another EEA country with no requirement for additional transfer tools or conditions or authorizations from data protection regulators in the EEA. The Commission has the power granted to it under Article 45 of the General Data Protection Regulation (GDPR) to adopt an adequacy decision in relation to a third country based on a comprehensive analysis of the third country’s laws and practices.
Appropriate safeguards have also been implemented with our third party service providers and partners. Further details, along with our Standard Contractual Clauses, can be provided upon request.
Appropriate safeguards have also been implemented with our third party service providers and partners. Further details, along with our Standard Contractual Clauses, can be provided upon request.
Use by minors
Our websites and online services are not intended to be used by anyone under the age of 18.
Updates
We may update this Privacy Notice Policy from time to time in response to changing legal, technical, or business developments. When we update our Privacy Notice Policy, we will take appropriate measures to inform you with the significance of the changes we make. We will obtain your consent to any material Privacy Notice Policy changes if and where this is required by applicable data protection laws. This Privacy Notice Policy was last updated as of the "Last Updated" date shown above.
Contact us
If you have any questions or concerns about our use of your personal information, please contact our data protection officer using the following details: - DPO_EU@celltrion.com (if you live in the EU/EEA); or DPO@celltrion.com (non-EU/EEA)
You also have the right to file a complaint with your local data protection authority: (such as https://edpb.europa.eu/about-edpb/board/members_en for EEA residents).
Cookies policy
Introduction
This Cookies Policy (the "Policy") explains how Celltrion Inc, the data controller, whose registered office is at Incheon, Republic of Korea (hereinafter "we", "our" or "us") uses cookies and similar technologies to recognize you when you visit this website. It explains what these technologies are and why we use them, as well as your rights to control our use of them.
Cookies
Cookies are a standard feature of websites that allow us to store small amounts of data on your computer about your visit to our Site. Cookies help us learn which areas of the Site are useful and which areas need improvement.
Use of Cookies
We use cookies in order to enable and facilitate the use of the website, for example to optimize the presentation or display. A distinction is made between required cookies for technical reasons and analytical cookies.
You can refuse or accept cookies from the Site at any time by activating the settings on your browser. Please be aware that if cookies are disabled, your experience on the Site may be diminished, and not all features of the Site may operate as intended.
We use cookies, such as:
GA4. GA4 is an analytical cookie and captures visitors’ behavior on the site. This cookie stores information about how users use the microsite, such as how users got to the microsite, the pages users visit and how long users spend on each page.
Third party cookies. Certain cookies are placed by a third party, for example YouTube by default sets a tracking cookie for marketing purposes when you embed YouTube hosted video, this is a third party cookie. The YouTube embedded player cookie uses the views of the embedded YouTube content to influence the viewer's browsing experience on YouTube.
To the extent any Personal Data is collected through cookies or similar technologies, the other sections of the Privacy Policy apply.
Contact Us
If you have any questions about our use of cookies or other technologies, please email us at:
- DPO_EU@celltrion.com (if you live in the EU/EEA); or
- DPO@celltrion.com (non-EU/EEA)